A 30 YR OLD MALE PATIENT WITH WEAKNESS OF RIGHT UPPER LIMB AND LOWERLIMB
MEDICINE CASE DISCUSSION
This is an online E logbook to discuss our patients deidentified health data shared after taking his/her/guardians signed informed consent.Here we discuss individual patients problems through a series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current based evidence based inputs.This elogbook also reflects my patient centred online learning portfolio and your valuable comments on comment box is welcome.
MAY 19 ,2021
A 30 YEAR OLD MALE PATIENT WITH WEAKNESS OF RIGHT UPPERLIMB AND LOWERLIMB ,DEVIATION OF MOUTH TOWARDS LEFT :
S.SHIVANIREDDY
MBBS 8th SEMESTER
ROLL NO 116
Under the guidance of Dr.VINAY(PG) AND Dr.VILASITH(INTERN)
I have been given this case to solve in an attempt to understand the topic of ''patient clinical data analysis '' to develop my competency in reading and comprehending clinical data including history,clinical findings,investigations and come with a diagnosis and treatment plan.
CASE DISCUSSION
A 30 YEAR OLD MALE PATIENT LORRY DRIVER BY OCCUPATION CAME TO THE OPD WITH CHIEF COMPLAINTS OF
1. WEAKNESS OF RIGHT UPPERLIMB AND LOWER LIMB SINCE ONE DAY.
2.DEVIATION OF MOUTH TOWARDS LEFT SINCE ONE DAY.
HISTORY OF PRESENTING ILLNESS:
Patient's brother was in jail since 2 months so that patient was emotionally disturbed about this situation.He went out and asked for money required for the bail for which he went in hot climate for 10-15 days.Patient was occasionally alcoholic who used to drink 500ml ofalcohol (whiskey) once in a week.Patient went to his relative's house(where fall has occured).Previous night before his fall he didn't drink.
Patient was apparently asymptomatic yesterday morning then he had:
suddenfall without loss of consciousness.
no complaints of involuntary movements and frothing
no complaints of involuntary micturition and defecation
no complaints of headache and blurring of vision
no complaints of chest pain ,palpitations ,syncopal attacks
no complaints of orthopnea,Shortness of breath and paroxysomal nocturnal dyspnea
HISTORY OF PAST ILLNESS:
Patient had no history of similar complaints in the past.Patient had road traffic accident 4 years back then he had posterior dislocation of shoulder,zygomatic and mandibular process.Patient had no history of diabetes, epilepsy,TB,Asthma,Hypertension
TREATMENT HISTORY:
No significant drug and surgical history
PERSONAL HISTORY :
Diet: Vegetarian
Apetite: Normal
Sleep: Adequate
Bowel and bladder movements:Regular
Addictions: Ocassional alcoholic(Weekly once-90 to 180ml/day)
Allergies: None
FAMILY HISTORY:
No significant family history.
GENERAL EXAMINATION:
The patient is conscious,coherent and not cooperative .He is drowsy and disoriented to time,place and person.
No pallor
No icterus
No clubbing
No cynosis
No generalised lymphadenopathy
No bilateral pedal oedema.
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM:Normal vesicular breath sounds heard
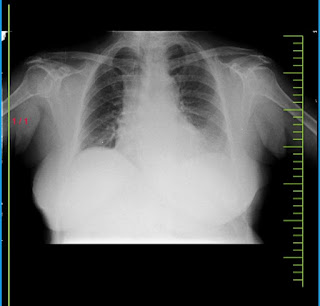
CVS:S1 and S2 heard.No added murmers.
PER ABDOMEN:Soft and non tender.No organomegaly.
CNS:
1.The patient is conscious,coherent and not cooperative .He is drowsy and disoriented to time,place and person.Patient shows no signs of meningeal irritation.
2.GCS :E4V4M6-14/15
3.REFLEXES : LEFTSIDE-Withdrawl reflex.
:RIGHTSIDE -Extensor reflex
4.PUPILS:
RIGHT :Dilated -Non reactory to light
LEFT : Normal- Reactory to light
LOCAL EXAMINATION: No External injuries or scars are seen.
INVESTIGATIONS:
1.HEMOGRAM
2.LIPID PROFILE
3.RANDOM BLOOD SUGAR:
4.LIVER FUNCTION TESTS:
6.APTT TEST:
7.PROTHROMBIN TIME:
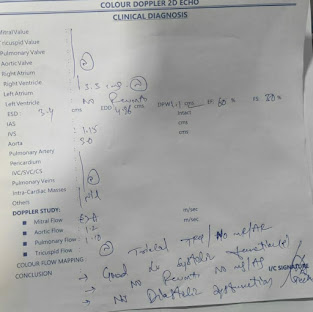
8.COLOUR DOPPLER 2D ECHO:
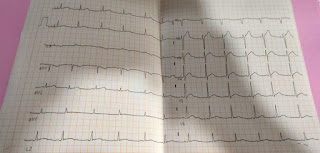
9.ECG
10.MRI SCAN:












Comments
Post a Comment