S.SHIVANI REDDY 116
32 yr old with CLD secondary to alcohol
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 32 year old male presented to the opd with C/O Yellowish discoluration of eyes and passage of dark yellow coloured urine since 1 month.
HOPI
Patient was apparently asymptomatic one month ago then he went to village for some occassion and had developed fever and was tested dengue positive and was also diagnosed to be ?liver failure ( Total bilirubin- 5gm/dl) . 3 days later after getting back from the village he was taken to miryalaguda and that his total bilirubin was 10 gm/dl for which he was given some medication and alcohol abstinance, but the patient continued drinking . He also used herbal medication for 1 week as he developed itching all over the body he stopped taking the herbal medication.
He is married for 10 years, childless didn't get tested , significant alcohol history . Starting with white liquor around the age of 15-16 years it increased to cheap liquor / whisky ,daily intake of around 180 - 360 ml . H/o alcohol abstinance 2 years back for 1 year and resumed drinking last year . H/o smoking from the age 25 years , daily used to smoke 4 cigarette s. He stopped smoking since the last 4 years .
Past history
Not a k/c/o DM , HTN, ASTHMA , EPILEPSY , TB , CAD.
PERSONAL HISTORY
Occupation - welding work in reddys laboratory.
Diet - Mixed diet
Appetite - Normal
Bowel and bladder - Regular
Sleep - adequate
Addictions -
Consumes alcohol regularly around 180- 360 ml.
H/o smoking from the age 25 yrs around 4 to 5 cigarettes/ day. He stopped smoking since the last 4 years .
No significant family history.
GENERAL EXAMINATION
Patient is conscious , coherant , cooperative .
ICTERUS - present
pallor present, cyanosis , clubbing , lymphadenopathy, edema .
VITALS
TEMP - 98.6 F
BP - 100/70 MMHG
PR - 82/ MIN
RR - 16 /MIN
SPO2 - 98 % ON RA.
SYSTEMIC EXAMINATION
CVS - S1, S2 +
RS - BAE + , NVBS
P/A -
- SHAPE OF ABDOMEN - OBESE
- ALL QUADRANTS MOVING EQUALLY WITH RESPIRATION.
- NO SCARS AND SINUSES
- HERNIAL ORIFICES ARE FREE.
- Mild Hepatomegaly is present
- SPLEENOMEGALY IS PRESENT
- NO HEPATOMEGALY
- BOWEL SOUNDS +
CNS
HMF - INTACT
CRANIAL NERVES EXAMINATION - NORMAL
SENSORY SYSTEM- INTACT
MOTOR SYSTEM EXAMINATON - NORMAL
CEREBELLAR EXAMINATION
FINGER NOSE COORDINATION - PRESENT
KNEE HEEL COORDINATION - PRESENT
PROVISIONAL DIAGNOSIS
Chronic liver disease secondary to ? Alcohol
INVESTIGATIONS
13/11/21
CBP
HB- 10.2
TLC - 7800
PLT - 1.57
LYMPHOCYTES - 12
LFT
TB- 15.9
DB - 7.10
AST - 366
ALT - 71
ALP - 358
TP- 7.2
ALB- 3.0
A/G - 0.71
CUE
COLOR - BROWNISH
APPERANCE - CLEAR
ALBUMIN - TRACE
SUGARS - NIL
BILE SALTS - NIL
BILE PIGMENTS - NIL
PUS CELLS - 2-4
EPITHELIAL CELLS - 1-3
RBC - NIL
BLOOD UREA - 12
S. CREAT- 0.5
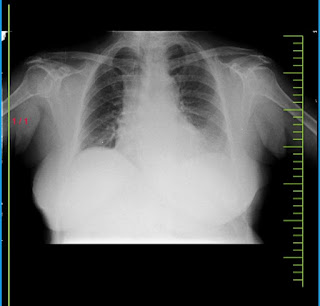
Chest xray PA view



Comments
Post a Comment