A 60 year old male presented to the opd with fever and right lowerlimb swelling.
- Get link
- X
- Other Apps
SHIVANI REDDY 116
▼
GENERAL MEDICINE CASE
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
A CASE OF 40 YEAR OLD WITH FEVER AND SOB AND RIGHT LOWERLIMB SWELLING since 3 days
A 60 year old male patient from Dhamera village came to casuality with chief complaints of
1) Fever since 3 days
2)SOB grade 2----> 4 since 2 days
3)Right lowerlimb swelling and redness since 1 day.
HOPI
Patient was apparently asymptomatic 3 days back and then he developed fever which was low grade, intermittent, relieved on taking medication and not associated with chills and rigor.
He has SOB(grade2 which progressed to grade4) No orthopnea or PND or pedal edema or chest pain or palpitations.
.No history of injury/trauma to lowerlimb
.He applied ointment for leg pain over right foot and later he developed redness and swelling over right foot
With these complaints they went to outside hospital and on presentation to the outside hospital vitals spO2-74% on RA with BP 70/40 and decreased urine output. He was put on IV antibiotics and IV multivitamins, IV nebulisation, IV inotrope .CPAP support was done and saturations were maintained on CPAP. Patient condition and poorprognosis was explained to patient attendees. He was advised for hemodialysis.Patient attendees were not willing for investigations and management and wanted tO refer to our hospital.
So they were reffered to our hospital.
GENERAL EXAMINATION:
Patient was conscious,coherent and co-operative and well oriented to time,place and person.
No pallor, icterus, cyanosis, clubbing, koilonychia, lymphadenopathy, edema.
VITALS:
Temp - 100 F
PR- 104 bpm
BP- 100/70mmHg
RR- 28 cpm
SpO2- 97% at RA
SYSTEMIC EXAMINATION
CVS: S1, S2 heard
Respiratory: Decreased Bilateral air entry.
Bilateral crepts present in infraxillary and infrascapulararea.
P/A :soft and tender
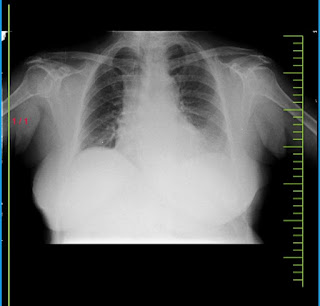
CLINICAL IMAGES
INVESTIGATIONS:
Cxr:
Diagnosis:
Sepsis secondary to right lower limb cellulitis
? Moderate ARDS (PaO2/FiO2= 100)
Pre renal AKI and ? Ischemic hepatitis
? Lumbar spondylosis (L2 to L5).
Treatment:
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat
To inj. PIPTAZ 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. PCM 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP > 65 MMHG
12. INJ. LASIX 20MG PO OD
Update: day 2
Post debridememt right Lower limb
Patient was intubated I/v/o type 1 respiratory failiure and Respiratory distress
Drugs used
Abg:
Ecg:
On 9/1/21
Day 3
S: NO fever spikes
O: pt intubated and is on mechanical ventilator
ACMV PC mode
Peep 7
Fio2 100
I:E 1:2
Pt is still on ionotropes noradrenaline @16ml/hr
Vasopressin @1.5ml/hr
Pt sedated and paralysed, on dexmedetomidine 10ml/hr
Atracurium 5ml/hr
intermittent regaining of consciousness
B/L pupil reacting to light
Bp : 100/70mmhg
PR : 82 bpm
Spo2 : 100% on fio2 100
Grbs:121
Cvs : s1s2+
Rs: b/L basal crepts +
P/A : soft,bs+
INVESTIGATIONS:
Treatment:
Rt feeds 200ml milk +free water 2nd hourly
IV fluids @75ml/hr
1. Propped up posture
2. O2 inhalation at 8 to 10 L/min
Maintain spO2 > 90%
3. BIPAP 4th hourly
4. Inj. PIPTAZ 4.5g /IV /stat
To inj. PIPTAZ 2.25g IV QID
5. INJ. CLINDAMYCIN 600MG IV TID
6. INJ. PAN 40MG IV OD
7. INJ. ZOFER 4MG IV BD
8. INJ. PCM 1G IV SOS
9. T. PCM 650MG PO TID
10. IVF NS and RL at U.O + 50 ml/hr
11. INJ. NORADRENALINE at 8 ml/hr to increase or decrease acc to MAP > 65 MMHG
12. INJ. LASIX 20MG PO OD
- Get link
- X
- Other Apps