A 50 yearold male with pain abdomen.
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box
A 50 year old male,labourer by occupation from Miryalguda came to casualty with complaints of pain abdomen since 2 days and was associated with nausea.
TIMELINE OF EVENTS:
6 years back:
Patient was apparently asymptomatic 6 years back until he lost his wife due to which he started drinking alcohol(90-180ml) everyday and used to do his routine work.
2years back:
Patient complained of tingling sensation on both upper and lower limbs for which he was taken to local hospital.Incidentally creatinine was raised to 2.4 mg/dl and since then he was on medication and stopped since one year.
2 days back:
Patient complained of squeezing type of abdominal pain which was sudden in onset.It was continuous, non radiating and was associated with nausea.It was aggravated on taking liquids and in supine position and releived on bending forward.He was taken to a localhospital where his pain was releived after taking medication.He was put on nasogastric tube and gastric contents were collected.They referred him to our hospital.
1 day back:
He was referred to our hospital with burning sensation in epigastrium.Patient had 1 episode of vomiting which was bilious .Patient also had heaviness in the chest 1 day back.
No c/o fever, pain,cold ,cough.
PAST HISTORY:
Not a k/c/o DM,HTN,CAD,CVA, Epilepsy.
FAMILY HISTORY:
Patient relatives had similar renal problem.
GENERAL EXAMINATION:
On examination patient is conscious, coherent, cooperative
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema
VITALS:
Temp-98.4 degrees F
PR-94 Bpm
RR-19Cpm
BP:150/90mm Hg on admission
Spo2:96% at room air
GRBS-133 Mg%
Systemic examination:
Per abdomen:
Diffuse tenderness is present
Rs:
Bilateral air entry is present.
Normal vesicular breath sounds are heard.
CVS:S1S2+
CNS: Normal
Diagnosis -
Acute Pancreatitis
INVESTIGATIONS:
Hemogram:
Hb-17.3
Tlc-17,800
PCV-48.9
MCV-81.5
MCH-28.7
MCHC-35.2
RBC COUNT-3.03
Ptc-2.38
Normocytic normochromic anemia with neutrophilic leucocytosis.
Sr Amylase-71IU/L
Sr Lipase-28 IU/L
Serology:Negative
LFT:
T.bil-1.50
D.bil-0.7
SGOT:40
SGPT:44
ALP-174
T.protein-7
Albumin-4
A/G-1.38
CVE:
Specific gravity:1.010
Albumin:positive
Puscells:3-6
Epithelial cells:2-4
Bile salts:negative
Bile pigments:negative
Amorphous deposits:negative
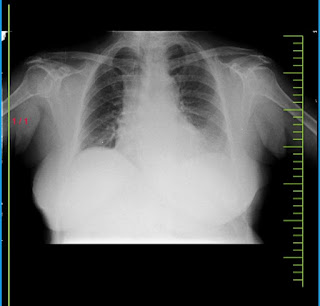
ECG:
CLINICAL IMAGES:
Acute pancreatitis
TREATMENT:
1)INJECTION CEFTRIAXONE 1g/IV/BD
2)INJECTION PAN 40mg IV/OD
3)NBM till further orders
4)IVF -125ml/hr
5)INJECTION ZOFER 4mg/IV/TID
6)THIAMINE 1 ampoule
100ml NS/IV/TID
7)Abdominal girth monitoring 4th hourly
8)BP/PR/RR /SPO2 charting





Comments
Post a Comment