Longcase:A 70 yearold male patient with SOB
LONGCASE -PRACTICAL FINAL EXAMINATION(70 yearold male with shortness of breath)
Hallticket no:1701006159
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients' clinical problems with the collective current best patient based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, and investigations, and come up with a diagnosis and treatment plan.
CASE PRESENTATION:-
A 70 year old male came to OPD with the
Chief Complaints of:-
-Shortness of breath since 20 days.
-Cough since 20 days.
History of presenting illness:
TIMELINE OF EVENTS:
Patient was apparently asymptomatic
20 days back:
Patient complains of
SHORTNESS OF BREATH:
*It was insidious in onset, gradual in progression- Grade 2
*Not associated with wheezing, No postural variation, No diurnal variation.
*No history of orthopnea and PND, Relieved on Rest.
COUGH:
*Cough is present on and off with sputum- *Mucoid in consistency,Not blood stained,Not foul smelling,No diurnal and nocturnal variation, It was relieved on medication.
*Loss of weight and loss of appetite is present.
*No history of fever,palpitations, chest pain, chest tightness,decreased urine output,syncopal attacks.
1day back:
Patient presented to the OPD with above complaints.
PAST HISTORY:
*Patient had similar complaints in the past and went to a local hospital where he was treated with intercostal tube drainage.
Patient had history of TB 10 years back and used medications for TB for 4 months.
Not a known case of Diabetes Mellitus Hypertension,Asthma and epilepsy
Family History:-
Not significant
Personal History:-
Diet:Mixed diet
Apetite:Decreased
Sleep: Adequate
Bowel and Bladder habits:Normal
Allergies:No
Addictions:-
Alcoholic since 50 years and Chronic smoker-smoked for 40 years-1chutta per day, stopped 10 years back.
General Physical Examination:-
•Patient is conscious,coherent and cooperative and well oriented to time, place and person.
•He is moderately built.
•Pallor:- Absent
•Icterus:-Absent
•Cyanosis:- Absent
•Clubbing :- Absent
•Lymphadenopathy:- Absent
•Edema:-Absent
Vitals:-
•Patient is afebrile
•Pulse rate:-82 bpm
•Blood pressure:-130/80 mm of Hg
•Respiratory rate:-28 cpm
•SpO2:-96% on Room temperature
•GRBS:-113mg%
Clinical Images:-
Systemic Examination:-It is done with consent if patient in sitting position in a well lit room .
Respiratory System:-
Inspection:
UPPER RESPIRATORY TRACT:
NOSE:-No DNS, polyps,turbinate hypertrophy
ORAL CAVITY-Poor oral hygiene
POSTERIOR PHARYNGEAL WALL:-Normal
LOWER RESPIRATORY TRACT:
Shape of the chest:-bilaterally symmetrical,Elliptical
Trachea:- Appear to be central
Apical impulse is not appreciated.
Chest Expansion:Decreased chest expansion on right side.
Chest Movements:Decreased ln rightside
No usage of Accessory muscles of respiration
No dilated veins,scars, sinuses.
No kyphosis/Scoliosis
Palpation:
All Inspectory findings are confirmed.
No local rise of temperature.
Trachea:- midline in position
Apical impulse is felt at the left 5th intercoastal space.
Tactile Vocal fremitus:- decreased on right side infrascapular and infraaxillary area
Chest circumference:- inspiration:- 74cm
expiration:- 75cm
AP diameter:21cms
Transverse diameter:25cms
Right hemithorax:-39 cm
Left hemithorax:-39 cm
•Dullness noted in right sided Infrascapular area and infraaxillary area
•Done on both sides in the following areas:-
-Supraclavicular-resonant on both sides
-Infraclavicular-resonant on both sides
-Mammary-resonant on both sides
-Axillary-resonant on both sides
-Infraaxillary-Stony dull note on right side, Resonant on left side
-Suprascapular-resonant on both sides
-Infrascapular-Stony dull note on right side , Resonant on left side
-Upper/mid/lower interscapular-Resonant on both sides
Auscultation:-
Done on both sides of the chest.
*Bilateral Air Entry:- Present
*Decreased Air Entry on Right Infrascapular and Infraxillary area
*Vocal Resonance:- Decreased on Right Infraxillary area
*No added sounds.
Abdomen Examination:-
Inspection:-
Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
Palpation:-
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
Percussion:-
There is no fluid thrill and shifting dullness.
Auscultation:-
Bowel sounds are heard.
Cardiovascular system Examination:-
Inspection:-
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse and pulsations cannot be appreciated
Palpation:-
Apical impulse is felt on the left 5th intercostal space 1cm medial to mid clavicular line.
No parasternal heave, thrills felt
Auscultation:-
S1 and S2 heard , no added thrills and murmurs heard.
Central nervous system:-
Higher Mental Functions:-
Patient is Conscious, well oriented to time, place and person.
All cranial nerves:-intact
Motor system:-Intact
Superficial reflexes and deep reflexes:-present and normal
Gait:- normal
No involuntary movements
Sensory system:-All sensation(pain, touch, temperature, position, vibration sense)are well appreciated.
Provisional Diagnosis:- Right sided Pleural Effusion secondary to Tuberculosis.
Investigations:-
Complete Blood Picture:
ULTRASOUND:
*Right moderate pleural effusion
*Bliateral minimal consolidatory changes in chest
CHESTXRAY:


















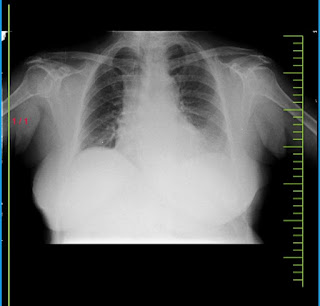
Comments
Post a Comment