Shortcase-A 60 yearold female with decreased urine output.
SHORT CASE(PRACTICAL FINAL EXAMINATION)
Hallticket no:1701006159
A 60 yearold female patient with reduced urine output.
This an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients' clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
CASE PRESENTATION
A 60 year old female patient came to OPD with the complaints of
Reduced urine output since 7 days
Shortness of breath since 7 days
History of presenting illness:
4years back:
Patient was apparently asymptomatic 4 years back when she developed high grade fever for which she visited a local hospital and was diagnosed with UTI.Patient was advised for some surgery but patient denied it and was on conservative treatment.
She also had joint pains for which she was given NSAIDs
7 days back:
Patient was admitted to our OPD with
*decreased urineoutput
*SOB which was grade 2 in nature
*Complains of fever of lowgrade ,intermittent in nature and releived on medication.
*No history of chills ,rigor and pedal edema
Past history:
Patient had similar complaints in the past since 3 years
Not a known case of Diabetes mellitus, Epilepsy, Cardiovascular diseases,asthma and tuberculosis.
Past surgical history:
4 years back patient had hysterectomy for prolapsed uterus.
Past drug history:
Patient took NSAIDS for 4 years.
Family history:
Not significant.
Personal history:
Diet: Mixed diet.
Apetite:Normal
Sleep: Adequate.
Bowel habits:regular
Bladder habits:decreased urine output
No allergies and addictions.
Examination was done after taking consent from the patient.
General examination: Patient is conscious, cooperative and well oriented to time, place and person. She is moderately built.
Pallor is present.
No signs of icterus, cyanosis, clubbing. lymphadenopathy and edema are present.
Vitals:
Patient is afebrile
Pulse rate: 90 bpm
Blood pressure: 110/70 mm of Hg
Respiratory rate:18 cpm
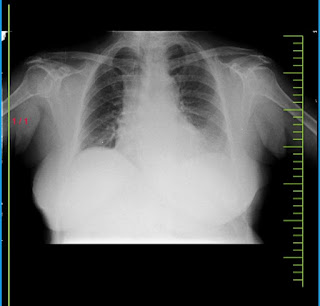
Clinical images:
Systemic examination:
ABDOMINAL EXAMINATION:
Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
There is no fluid thrill , shifting dullness.
Percussion over abdomen- tympanic note heard.
Bowel sounds are heard.
CARDIOVASCULAR SYSTEM:
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
Apical impulse and pulsations cannot be appreciated
Apical impulse is felt on the left 5th intercostal space 1cm medial to mid clavicular line.
No parasternal heave, thrills felt
S1 and S2 heard , no added thrills and murmurs heard.
Chest is bilaterally symmetrical
Trachea – midline in position.
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
The following areas were percussed on either sides-
Supraclavicular
Infraclavicular
Mammary
Axillary
Infraaxillary
Suprascapular
Infrascapular
Upper/mid/lower intersacapular
All are resonant
AUSCULTATION:
Normal vesicular breath sounds heard
No adventitious sounds heard.
CENTRAL NERVOUS SYSTEM EXAMINATION.
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system: Intact
Superficial reflexes and deepreflexes are present
Gait is normal
No involuntary movements
Sensorysystem- All sensations (pain, touch, temperature, position, vibration sense) are well appreciated.
PROVISIONAL DIAGNOSIS:Acute kidney injury on chronic kidney disease.
INVESTIGATIONS:
Hemogram:
Hemoglobin: 7.7 gm/dl
RBC count: 2.77 millions/cumm (3.8-4.8)
Total Leucocyte Count: 5800 cells/cumm
Lymphocytes: 17 (20-40)
Complete urine examination:
Blood urea:
Serum creatinine:Serum Iron:Ultrasound :
1)Grade 1 RPD in right kidney
2)Grade 2 RPD changes in left kidney
3)Bilateral cortical cysts
Treatment:
Tab. LASIX 40 mg PO BD
TAB. NODOSIS 500mg PO BD
TAB. OROFER XT PO BD
TAB. PAN 40mg PO OD
TAB. ULTRACET 1/2 TAB PO QID
INJ. IRON SUCROSE 1Amp in 100 ml NS ONCE WEEKLY
INJ. EPO 5000IU/SC/OD
SYRUP. CRANBERRY 15ml PO TID









Comments
Post a Comment