A 19Y/M with fever thrombocytopenia
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
A 19year old male came to the opd with complains of fever since 1 year.C/O SOB since 15 to 20 days
HOPI:
Patient was apparently asymptomatic 1 year ago then he developed lowgrade intermittent type of fever which aggravated since 15 days, mainly during the night time,temporarily relieved on medication.It was associated with bodypains and headache, low backache.Not associated with cold and cough, burning micturition and rash on body.He complains of SOB since 15 days which is present even on rest,which aggravates after having food.Bloating and chesttightness are present.
Patient complains of bleeding gums since 2 days
Cold is present since 3months after drinking softdrinks/colditems.
PAST HISTORY
N/K/C/O DM, TB, epilepsy, CVA, CAD, thyroid disorders and bronchial asthma.
FAMILY HISTORY:
Not significant
PERSONAL HISTORY:
Diet :Mixed
Apetite:Normal
Bowel and bladder Movements:Regular
Sleep:Adequate
No allergies and addictions.
Daily routine: Patient wakes up at 7AM and has some breakfast at 8:30AM and goes to college at 9AM.He skips his lunch.He comes back from college at 5 PM and eats some food at 6:30PM.He goes to play till 8pm.He skips dinner.He studies till 10pm for 2 hours.He sleeps by 11am.
He goes to college regularly despite his fever but 15 days back he could not eat properly due to SOB while eating.
His dailyroutine is not changed due to his symptoms.
Course in the hospital:
Patient came with above complaints and necessart nivestigations and thorough clinical examination was done.
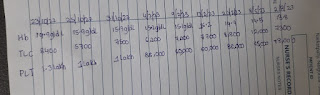
Hemogram was done on 2/8
Hb :13.8mg/dl
plateletcount:78000lakhs/cumm
Widal test,rapid dengue test,blood for MP strip test was done .They are negative.Blood,urine and sputum was sent for culture and sensitivity.It showed no growth.
Sputum was sent for CBNAAT.MTB was not detected.
On monitoring temperature ,feverspikes were not seen .It was lowgrade fever.Patient was complaining of backpain.Dorsal spine xray was done.It was normal.Patient was complaining of bleeding gums since 2 days.His platelets trends were fluctuating.
Peripheral smear was done .It showde giant platelets.
Hemogram was repeated on 6/8/23
Hb:14
Plt count:68000lakhs/cumm
6 minute walk test was done:
Before 6min walk test
Spo2-99 %
RR-20 cpm
PR-75 bpm
BP-100/70 mmHg
After 6min walk test
Spo2- 98 %
RR-22cpm
PR-78bpm
BP-100/80 mmHg.
Patient was diagnosed with immunethrombocytopenia and symptomatic treatment was started.
Platelet trends :
GENERAL EXAMINATION:
On examination patient is conscious, coherent, cooperative
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema
VITALS:
Temp-Afebrile
PR-64bpm
RR: 22Cpm
BP:110/70mm Hg
Spo2:99% at room air
GRBS charting: 98mg/dL
Systemic examination:
Per abdomen:
Soft,Nontender
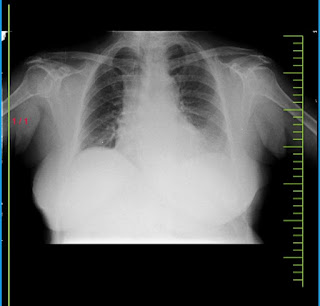
RS:
bilateral air entry is present.
Normal vesicular breath sounds are heard.
CVS:
S1S2 heard.No murmurs
CNS:
HMF+,NFND
Provisional Diagnosis:
IMMUNE THROMBOCYTOPENIA
Investigations:
Hemogram:(2/8/23)
Serology:negative
BGT:B+ve
RBS:79mg/dl
Widal test: negative
Rapid dengue:negative
Blood for MP strip test:negative
CBNAAT:MTB not detected
Blood/urine/sputum culture: No growth is detected
PT:17sec
APTT:35sec
INR:1.2
PLBS:114mg/dl
FBS:80mg/dl
HBa1c:6.4mg/dl
CRP:negative
Clinical images:
Treatment:
1)Tab Dolo 650 mg/PO/TID
2)Monitor vitals 4 th hourly

















Comments
Post a Comment